A partnership between Raven Capital, the Lawson Foundation, and the federal government leverages an impact-investing strategy from the clean energy sector to tackle the diabetes epidemic in Indigenous communities.
Melody Hyde Swan works on the front line. She is a registered dietitian and is serving her fifth year as a health promotion coordinator at Abegweit First Nation, out of an office in Scotchfort, Prince Edward Island, adjacent to the community. Jacques Cartier landed on the island in 1534; its original residents have been living with colonization longer than most Indigenous Peoples in Canada.
Abegweit is the Miꞌkmaq name for Canada’s only provincial island and is translated as “cradled by the waves.” The province’s two First Nations, Abegweit and Lennox Island, which is located 141 kilometres west down the Veteran’s Memorial Highway, have some of the smallest on-reserve populations in Canada. Only 35 people currently live in Morell 2, one of the three reserves that make up Abegweit (the others are Rocky Point 3 and Scotchfort 4).
Swan hosts walking clubs and healthy breakfasts and coordinates one-on-one counselling and a variety of other services that help people lead healthier lives. “I love my job right now because it is connecting people with the basics of food,” she says. Delivering healthy food boxes became a big part of her day as the community adjusted to life during the pandemic and Swan found immediate benefit in terms of developing healthy shopping and eating habits, and having personal contact either over the phone or safely distanced.
She doesn’t think the food box program will be funded beyond its current emergency pandemic life. Even if something is working or shows potential, she says, there is no guarantee the government will continue to provide funding.
Swan talks wistfully about a community garden initiative that was started a little over three years ago. “The community garden was free for people to take from and grow whatever they wanted. They had just really broken ground into getting all ages involved. We had the daycare, the youth group. We were just getting people into the harvesting and we had to shut down. The funding ran out.”
The community garden was free for people to take from and grow whatever they wanted … We were just getting people into the harvesting and we had to shut down. The funding ran out.
Melody Hyde Swan
There’s a direct link between legal or bureaucratic restrictions on nutritious local food and the diabetes epidemic that has crippled so many Indigenous communities in recent decades. When asked why diabetes has been so devastating, Swan takes a long pause and says the question is too big. Finally, she offers a few reasons: “Past trauma from everything from colonization, from residential schools and how that relates to food and our relationship to food, a lot of emotional eating and a lot of control with food…”
However, Swan and the members of Abegweit First Nation are looking to take back that control through their partnership in an innovative Indigenous-led impact-investing venture, backed by Raven Capital and the Lawson Foundation, that’s focused squarely on short-circuiting the scourge of diabetes in remote communities.
***
According to Diabetes Canada, “Indigenous Peoples are diagnosed with diabetes at a younger age, have more severe symptoms when diagnosed, face higher rates of complications and experience poorer treatment outcomes.” A 2020 study by the First Nations Health and Social Secretariat of Manitoba and the Manitoba Centre for Health Policy found that First Nations children in that province are a staggering 25 times more likely to be diagnosed with type 2 diabetes than non-Indigenous children.
The impact of diabetes on health cannot be understated. It is ranked among the top 10 killers in the world, although it could be number one, as it is a factor in every other illness on the list, including heart attack, stroke, cancer, and kidney disease. The pandemic highlights this deadly connection. “Among people with diabetes the mortality rate was 7.3%,” the American Diabetes Association reported, “more than three times that of the overall population.”
The economic burden is also clear. A 2017 literature review by the Institute of Health Economics, Diabetes Care and Management in Indigenous Populations in Canada, identified “systematic breakdowns along the entire care pathway for many Indigenous Peoples with diabetes. As a result, care is often reactive and episodic, with Indigenous patients experiencing comparatively high rates of emergency interventions and hospitalization, which are key drivers of health care costs for Indigenous Peoples with diabetes.” The report noted that in Manitoba, the estimated per capita health cost for a First Nations person living with diabetes is $3,656, versus a First Nations person without diabetes at $1,359. Similar cost differences were found in Saskatchewan.
***
Food has been a fundamental tool in colonization in North America. The extermination of the buffalo was one of the most brutal expressions of this tool of genocide. Nations were imprisoned on tiny tracts of land cut off from traditional territories and waters. Hunting, fishing, and harvesting were criminalized and enforced with the well-documented institutional racism of the Canadian justice system. Children were forcibly taken from their homes and traditional diets and then starved in the residential school system.
Independence was brutally replaced by government dependence and dominance. Throughout generations, freedom fighters, language keepers, rights defenders, and ceremony and artistic practitioners kept the fires of the Nations burning.
In recent years, however, First Nations have been taking back control of their communities from a system of government-managed poverty that has been enforced ever since the Indian Act came into effect in 1876.
Community-driven efforts have been taking over institutions once controlled completely by the government, including education, economic development, band management, and health. The Indigenous renaissance is evident not only in self-government, but also in the emergence of Indigenous arts and culture in mainstream Canadian society, as well as in language and ceremony in our homes and communities. In fact, leaders in this emerging Indigenous generation are taking control in many sectors and changing the game.
Among this group is Jeff Cyr, who is Métis and the managing partner at Raven Indigenous Capital Partners, which was founded in 2018 to facilitate the flow of capital through impact investing to support the ongoing revitalization of the Indigenous economy in Canada. Raven Capital currently runs a $25-million Indigenous Impact Fund, has brought to market a first-of-its-kind social finance instrument ($5.1 million), and is preparing to launch a much larger $25-million Indigenous Diabetes Reduction Bond.
Raven traces its roots to 2015 and the first Indigenous Innovation Summit in Winnipeg, which Cyr helped co-create. During this event and a subsequent summit in 2016, Raven connected with Aki Energy, which had faced increasing barriers to success because of the ways in which public funding flows to projects, in particular in the clean energy space. During the 2016 summit, the McConnell Foundation sponsored a solutions lab session to address these barriers and change the old funding models. The upshot was the development of geothermal energy projects in three Manitoba First Nations: Sagkeeng, Peguis, and Fisher River.
“We started looking at alternative funding methodologies around clean energy on First Nations,” Cyr says over the phone from Raven’s West Coast office. “Geothermal is capital-intensive to put in but gives you massive environmental and energy savings,” he explains. “The upfront capital costs were seen as a significant roadblock, and [the Department of] Indigenous Services’ notorious red tape meant that the project was either not going to get off the ground or was built to fail.”
In launching the project, Raven pioneered what it calls a “community-driven outcomes contract” (CDOC), with an eye to installing an initial 125 residential geothermal units in on-reserve housing, with an eventual goal to operate at scale (the plan is to install more than 500 units in total). The basic principle behind CDOCs is to develop a costing model that begins not with profit but rather a full accounting of the desired outcomes for the community – employment and training, reduced emissions, lower energy bills, and avoided social assistance costs, as well as the capital required to build these projects. Raven then secures an outcomes buyer, typically a federal or provincial government, that agrees to “pay for success” of the achieved outcomes. Then Raven raises the necessary funds through private capital, as well as from philanthropic organizations, promising a return of 4% interest for investors. As an explainer on Raven’s website illustrates, a $1-million outcomes contract, for example, yields $1.2 million for the investors, but the total economic value of the outcomes – clean energy, new jobs, et cetera – amounts to $1.8 million.
The communities in the Island Lake region and the Lawson Foundation … approached us and said, ‘Can we use your financing method to address type 2 diabetes in our communities?’ Because it is a crisis, it is an epidemic.
Jeff Cyr
The use of these new energy funding models raised intriguing possibilities about new ways of tackling diabetes. “The communities in the Island Lake region and the Lawson Foundation have been working on food security and food sovereignty issues for a while in Manitoba,” says Cyr. “They approached us and said, ‘Can we use your financing method to address type 2 diabetes in our communities?’ Because it is a crisis, it is an epidemic.”
In response, Raven teamed up with the Lawson Foundation and the Government of Canada to bring this impact-investing approach to bear on food security and health issues. “We have been doing some of this work for over 30 years, and everyone sees the numbers keep going up higher and higher,” says Lawson CEO Marcel Lauzière with a heavy sigh. “There is research that shows that as a 20-year-old Indigenous person, you have an 80% chance of getting type 2 diabetes.”
In September 2019, Raven convened a two-day “Indigenous solutions lab” in Winnipeg (the first of a series of four labs), with health experts and representatives of six First Nations in PEI and Manitoba in attendance. Participants hashed out ideas on how to connect healthy living principles, Indigenous knowledge, local food production, and home-grown approaches to wellness as a way of plotting a five-year path for reducing diabetes and all the conditions associated with this chronic disease.
“Why we are so interested in the community-driven-outcomes contract is that it starts at the community level,” says Lauzière. “It is not the government. It is the community that decides what issue it wants to address. It decides on the interventions that it wants to develop to address those issues.”
The emerging partnership, which includes the federal government, is meant to leverage more investment: “Let’s find some investors who believe in this approach and who will invest in the intervention,” Lauzière says. “Give us the dollars to deliver them. Let’s show the results to the federal and provincial governments, who are paying ridiculous amounts of money to address these issues, and they will see the savings and they will reimburse the investors, who will then continue to invest in this approach. It is community-driven and ground-breaking – there is nothing [like it] that exists anywhere else.”
Why we are so interested in the community-driven-outcomes contract is that … it is the community that decides what issue it wants to address. It decides on the interventions that it wants to develop to address those issues.
Marcel Lauzière
The strategy seems to be working. Earlier this year, Raven announced it had secured a US$506,000 grant from the World Diabetes Foundation. “The grant will fund the development and launch of a pilot Diabetes Reduction Bond/Community-Driven Outcomes Contract (CDOC) to finance the diabetes prevention interventions created by the Lab,” according to a press release from Raven. “The CDOC will cover a 5-year intervention period, bringing in private capital through the Bond and placing government in a position to pay for successful outcomes. The initial CDOC will focus on reducing or preventing type 2 diabetes in 6 Indigenous communities.”
On March 8, 2021, just weeks after Raven revealed that investment, the Lawson Foundation announced that for the next 10 years, it will use an impact-investing approach to fight type 2 diabetes in northern and Indigenous communities, working with leaders like Cyr.
“We have been proactive on the diabetes front because we have some experience there and connections with some Indigenous communities,” says Lauzière. “We were an early funder of the Kahnawake diabetes-prevention school program in the early 1990s, and it still continues and has had impact around the world.”
In addition to such projects, Lawson’s investment is an expression of the foundation’s commitment to reconciliation. “Five years ago, when the [Truth and Reconciliation Commission report] came out, we signed on to a philanthropic declaration around reconciliation,” Lauzière says. “We have been working on that and how it can inform everything we do. For the next decade, the focus of our diabetes-prevention strategy will be on Indigenous northern and remote communities. Working with Indigenous advisors, all of our funding for this strategy will be focused on that.”
We have to rethink how we address social problems in order to make lasting change in our communities. Indigenous communities and knowledge have to be at the centre of the approach.
Jeff Cyr
Cyr expands on this idea. “We have to rethink how we address social problems in order to make lasting change in our communities. Indigenous communities and knowledge have to be at the centre of the approach. This solution really is a trifecta that will drive transformation in the healthcare system: the investment of private capital allows Indigenous community-led intervention to improve health outcomes, which results in massive systemic savings for government.”
The entire approach offers a stark contrast to the normal government response to the diabetes war, which has been to provide battlefield medical support. “There is a fundamental recognition here that the healthcare system, which is run by the province primarily but funded by the federal government for Indigenous Peoples on reserve, is really a reactive system,” says Cyr. “It is largely focused on responding to a symptom through clinical measures – dialysis, amputation, pharmacology – rather than through prevention.”
He says the diabetes-reduction bonds represent an alternative to a system that has utterly failed Indigenous people, in the form of “private capital coming in to fund an intervention based on the success, or what we call a ‘pay-for-performance’ model,” Cyr explains.
Raven’s mission, indeed, is to build relationships from the community outward, and it has found success using Indigenous philosophies, which are centred on developing personal connections. “Before we even started the lab,” says Cyr, “there was a five-month pre-engagement with the community – think town halls, open sessions, and that kind of stuff – to share and discuss if we had to do something, what would we do, and what has to be done in the community to bring about these changes.”
***
The two sets of communities participating in this experiment are separated by half the country and differ significantly in population. Some 3,200 kilometres west of the tiny Abegweit and Lennox Island First Nations on Prince Edward Island, the Manitoba fly-in communities of Island Lake, which boast an on-reserve population of nearly 7,500, are the four largest in Canada. As such, these First Nations are fitting pathfinders in the fight for a breakthrough in the diabetes war.
The story of diabetes in Indigenous communities actually begins in Atlantic Canada. Diabetes has been the result of colonization in the past and persists because of the ways of the corporate food industry in the present. “The way I view it, we’ve all been inflicted through colonization,” says Roseanne Sark over the phone from her home in Somerset, PEI. She has called in the evening after having to cancel our earlier interview to handle some “grandma duties.”
Sark is director of health for the Miꞌkmaq Confederacy of PEI, and she coordinates the efforts of the two First Nations on the Island. “Initially, the [Raven/Lawson] project was going to be out west in Manitoba,” she explains. “In terms of comparatives, with PEI being an island on the East Coast, it just seemed fitting. There are differences, but diabetes is diabetes.”
That relationship we had with Mother Earth pre-contact – we had that in us. We have that in us to ignite.
Roseanne Sark
The connection is present in the shared history of Indigenous communities and also a shared philosophy. “That knowledge – we as a people have had that relationship once before,” she says. “We knew what was in all the food that we ingested and that it was a gift that the Creator provided us. That relationship we had with Mother Earth pre-contact – we had that in us. We have that in us to ignite.”
Half a continent away, the communities of Island Lake are accessible only by plane, with the nearest airport 300 kilometres northwest in Thompson, which itself is at the end of Highway 6, about 800 kilometres from Winnipeg. Made up of four First Nations – Garden Hill, Wasagamack, Red Sucker Lake, and St. Theresa Point – Island Lake is served by an ice road that is open only during the coldest months of the northern Manitoba winter. (The History channel’s Ice Road Truckers series, about drivers and machines going to the extreme, documented an entire season of deliveries to Island Lake.) Despite the isolation, the impact of modern processed food and the loss of traditional eating habits has caused diabetic devastation in these communities.
Edward Flett is the director of health for Island Lake, a role he has held for nearly a decade. It took a couple of weeks of telephone tag, emails, and texts to finally nail down an interview. He is apologetic and explains that it is the end of the fiscal year, with so much going on and so much reporting to be done.
The pandemic has revealed another example of how the burden of Indigenous Affairs funding has made it difficult to respond in real time to an ongoing health crisis. In January 2021, the Island Lake region had the highest number of COVID-19 cases in the province, prompting a lockdown, state of emergency, and support from the Armed Forces.
Yes, there were additional funds sent to First Nations to respond to the pandemic, yet the duties that came with them, practical and financial, added a burden to an already overwhelmed system. “Our funding comes from Canada, and we were not able to deliver our community-based programs accordingly because of how the virus impacted our community,” Flett says. “The virus forced us to adjust our program requirements and service delivery.”
Indigenous Services Canada instituted a major shift in their arrangements with First Nations that will allow 10-year agreements. The nationwide transition includes Canada’s most notoriously archaic and convoluted pieces of constitutional law, one of the federal government’s most bloated bureaucracies, and 634 First Nations with a kaleidoscope of diversity in languages, cultures, land bases, and governance. Some First Nations have only dozens of residents, while others are home to tens of thousands. Some are in the suburbs of major cities and others in the most remote parts of this massive country. Implementing the new arrangements is, without hyperbole, a logistical nightmare.
“We have had to make a transition in the last couple of years on how we spend the money and the way we are supposed to report it,” says Flett. “This year, we are going to have to do some extra work because we have received funding from Health Canada to address the COVID expenses.”
He is particularly concerned with how his reporting on the mental health dollars for the past fiscal year are going to be received. In his community, like all communities, mental health services changed dramatically and sometimes desperately in response to isolation, outbreak, and the existential threat of a global pandemic. He calls his report “colourful,” and he hopes there is some understanding. An idea crafted in Ottawa has to be put into practice thousands of kilometres away, and then implemented and managed by local health directors like Flett.
Every year we have more and more type 2 diabetes coming up earlier than normal, and that is a big concern for us.
Edward Flett
Life under the pandemic has slowed the diabetes prevention project backed by Raven and scoped out during those solutions lab sessions two years ago. Flett, however, remains hopeful it will be implemented because diabetes continues to rage in his community. “Every year we have more and more type 2 diabetes coming up earlier than normal, and that is a big concern for us,” he says. “We did a study on kidney health. We did testing here in the community and found that a good number of people” – 30% – “are going to experience renal health problems within 10 years. That is a scary number. That is all related to diabetes.”
For Roseanne Sark, the discussion in the solutions lab has lit a spark. “We were able to talk about the challenges and the opportunities, look at best practices and areas where we can advance and make change. That type of environment puts people in that mindset. It is a matter of transferring that kind of collaboration or deliberation into the communities.”
Cyr relates how the communities in the Island Lake region want to see a change in the landscape as part of the fight against diabetes. “What was identified was a need for a physical space, which we are now calling a Healthy Hub – a centre in the community for education, cooking classes, preparation, a vertical grow-op, a micro abattoir and micro butchery where you can take traditional foods. These can be butchered in what is now going to be a Health Canada–certified micro-abattoir inside this centre. We would have never thought about that if we hadn’t asked the community.”
This approach also plays into how people meet and how they build relationships. “As a hunting and gathering society, we have fishing and we have hunting – we have those relationships,” says Sark. She wants to incorporate traditional philosophy into this new connection with Raven. “The leadership have led the way. They understand that we need to create relationships such as the one we have with Raven.”
Sark, in fact, sees the possibility of physical transformation. “Funding really does change the landscape of our communities,” she says. “If we can have a community garden, if we can have a greenhouse, if we can have those people who can educate about what is in the food, the nutrients, then we can make that shift.”
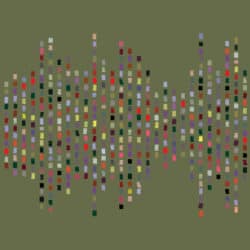
The artwork that accompanies this piece, Ketuimalgotmek, was created by Amanda Amour Lynx. They provided the following statement about the image:
Ketuimalgotmek explores childhood memories of spending time in grandma’s (Flora Robertson, née Isadore) garden in Montreal. I was taught how to tend to tomatoes and cucumbers, yielding so many fruits that the whole family would share over mealtime. I was taught the value of Lꞌnu storytelling via her acts of repetition and emphasis. “Remember when you gave me the hose?” she would say every visit, recalling when my five-year-old self accidentally pointed the hose in her direction and drenched her while I was watering her abundant garden. In this nature, she teaches about how we keep stories alive by retelling them, with humour and timing. If a story is told often enough, it becomes legacy.
The illustration features a Miꞌkmaq hieroglyph sourced from a grace-before-eating prayer. Hieroglyphs were our earliest recorded form of language, due in part to Jesuit missionaries converting prayers into Lꞌnuismk (Miꞌkmaq language). The use of language is an intentional act of revitalization, similar to my grandmother’s teaching about keeping stories alive. Lꞌnu artist, and fluent language speaker, Michelle Sylliboy’s notable cultural work in recontextualizing a hieroglyphic lexicon for Miꞌkmaq people inspires this piece. The lexicon serves to shift the emphasis of colonial pain from the prayer book influence, reclaiming our narratives and engagement with culture. I wanted ketuimalgotmek to highlight the empowerment in our communities as they develop new relationships with food and access, honouring netukulimk and msit noꞌkmaq by connecting story and language to foodways.
The repeated tomato motifs speak of these memories on top of textured 3D renderings using the program Cinema 4D, conveying a dreamlike space where plant knowledge connects with cosmology. The textural and colour elements envision star stories and plant stories, interwoven with embedded knowledge of the animacies of both. Fiddleheads (maꞌsusi) are featured as a traditional food source.