Introduction
Most of what influences our health comes from outside the formal health care treatment system (Raphael, 2009; Wilkinson & Marmot, 2003). There is also general recognition that the well-being of communities depends on numerous actors– especially nonprofit organizations—operating in many environments (Health Council of Canada, 2010). Unfortunately, there are significant health inequities that persist across different population groups in Canada and action to change this situation is long overdue (Johnson, Abonyi, Jeffery, Hackett, Hampton, et al., 2008). For example, a high proportion of First Nations people have higher diabetes rates than non-First Nations people (Loppie Reading & Wien, 2009) and people living on low incomes are 118% more likely to have heart disease than people living on higher incomes (Lemstra & Neudorf, 2008). It was these beliefs and facts that led a group of nonprofit, “community-based organizations” (as they are referred to in Saskatchewan) and government staff to come together to design a research project in 2009 with the two-fold purpose of: a) documenting the determinants of health being addressed by a sample of community-based organizations, and b) discerning how best to use the collected data as a catalyst for further collaboration and action. This article presents the results of this Regina Regional Intersectoral Committee1—Community Support Team (Regina RIC Team) research project.2
It is noteworthy that over the few years the Regina RIC Team had been meeting, it had grown more and more impatient about the apparent lack of co-ordinated action on the determinants of health, especially given that the welfare state was and still is undergoing restructuring in Canada. This restructuring has been characterized by a “shrinking state” approach (Burke, Mooers, & Shields, 2000), minimal government service provision, promotion of self-reliance and reliance on the informal sector (e.g., family and friends) to meet personal needs, increasing government expectations of the nonprofit sector and private sector to deliver more social services, and a reduction in citizen engagement by governments (Bakker & Scott, 1997; Broad & Antony, 1999; Brooks, 2001; Browne, 1996; Teeple, 2000). Despite the aura of pessimism presented by this list, the restructuring of the Canadian welfare state may not be wholly negative, as it may provide an opportunity for us to work toward a “solidarity-based model involving a new and clearly defined partnership” between governments and the nonprofit sector (Tremblay, Aubry, Jette, & Vaillancourt, 2002, p. 20).
Despite the many decades of restructuring, questions persist about who should be responsible for the design and delivery of which human services—especially given that many of these services are intended to meet basic human needs, which are in essence, determinants of health (Brock & Banting, 2001; Mulvale, 2001; Rice & Prince, 2003). Community-based organizations undertake numerous functions intended to create a healthier society (Danaher, 2011) and the sector as a whole acts as a “social seismograph” leading the way in identifying new social issues (Hall & Banting, 2000, p. 3), which are also health issues. Community-based organizations have always been an integral part of the human service system, but there appears to be no more consensus today than there was 70 years ago about who (i.e., community-based organizations, governments, private sector, families/friends) should deliver which services to whom (Canadian Welfare Council, 1938; O’Sullivan & Sorensen, 1988; Thériault, Gill, & Kly, 2002). In fact, Canadian scholars continue to lament the lack of an explicit, formal relationship between the nonprofit sector and governments regarding human services specifically and democracy generally (Brock, 2002; Elson, 2011; Phillips, 2009).
This study is not specifically about these government and community-based organization relationships, but rather, it is about the nature of community-based organizations’ services and how they contribute to creating healthier communities. This article examines the nature of community-based social services using a population health framework. This research is worthy because nonprofit social services are not often recognized for their health work (Hanlon, Rosenberg, & Clasby, 2007).
The Regina RIC Team adopted a population health framework to examine the determinants of health being addressed by nonprofit, social service organizations working with marginalized populations in Regina. Population health is “more than traditional public health” in that it encompasses determinants of health and their inequities (Young, 2005, p. 5). These inequities are exposed in research that shows a variety of marginalized groups have higher morbidity and mortality rates than others (Lemstra & Neudorf, 2008; Marmot & Wilkinson, 2006). Essentially, population health comprises a variety of health determinants that manifest themselves across different spheres (e.g., individual, community, state) which interact over time and space through many different processes of change (e.g., learning) that result in a variety of positive and negative health outcomes (Hancock, Labonte, & Edwards, 2000; Labonte, Muhajarine, Abonyi, Woodard, Jeffery, et al., 2002). Within this framework, there is recognition that the well-being of communities depends on a variety of actors (e.g., schools, food banks, emergency shelters).
The Regina RIC Team adopted the term “determinants of community well-being” to emphasize the non-medical nature of their research. In this research, “determinants of community well-being” is synonymous with “determinants of health” and are terms used interchangeably in this article. These determinants influence people’s health and include the following: income and its distribution, employment, education, social safety net, housing, food security, social inclusion, health services access, culture and early life (Bolen & Ramsay, 2008; Hancock, Labonte, & Edwards, 2000; Marmot & Wilkinson, 2006; Raphael, 2009). Community-based organizations tend to work where determinants of well-being and poor social conditions are prevalent (Hall & Banting, 2000; Shragge & Fontan, 2000). The Regina RIC Team believes—as do others—that if we strengthen the determinants of community well-being, we will generate more positive population health outcomes.
The nonprofit social service sector is of particular interest in this health research project. In general, these organizations are voluntary, nonprofit sector agencies that are institutionally separate from government and the private sector, have an organizational structure, exist to serve a public benefit, are self-governing, do not distribute profits to members, and depend on volunteers to varying degrees (Government of Canada, 2002; Hall & Banting, 2000). Nonprofit social service organizations, in particular, refer to a range of agencies that provide services to specific populations (e.g., people with mental health disabilities, people living on low incomes, single-parent families, people who have been released from corrections facilities) to promote their social, mental and economic well-being as well as protect and advance their human rights. The nonprofit social service organizations that participated in this study fall into the following International Classification of Nonprofit Organizations (ICNPO) categories outlined in Cornerstones of Communities (Hall, de Wit, Lasby, McIver, Evers, et al., 2004): social services, development and housing, and advocacy for human rights.
This study took place in Regina, Saskatchewan, but it has applicability to other cities in Canada because all cities have nonprofit sector organizations delivering social services. Even though each city has its own unique history and culture regarding the social service system, as well as a diversity of types of community-based organizations, some issues are common across the sector. For example, in their Canadian study, Hall, Andrukow, Barr, Brock, de Wit, et al (2004) explain many organizations’ funding sources are unstable, there is an increasing degree of importance placed on cross-agency collaboration, and there has been a decline over time in the number of volunteers serving on boards of directors.
Method
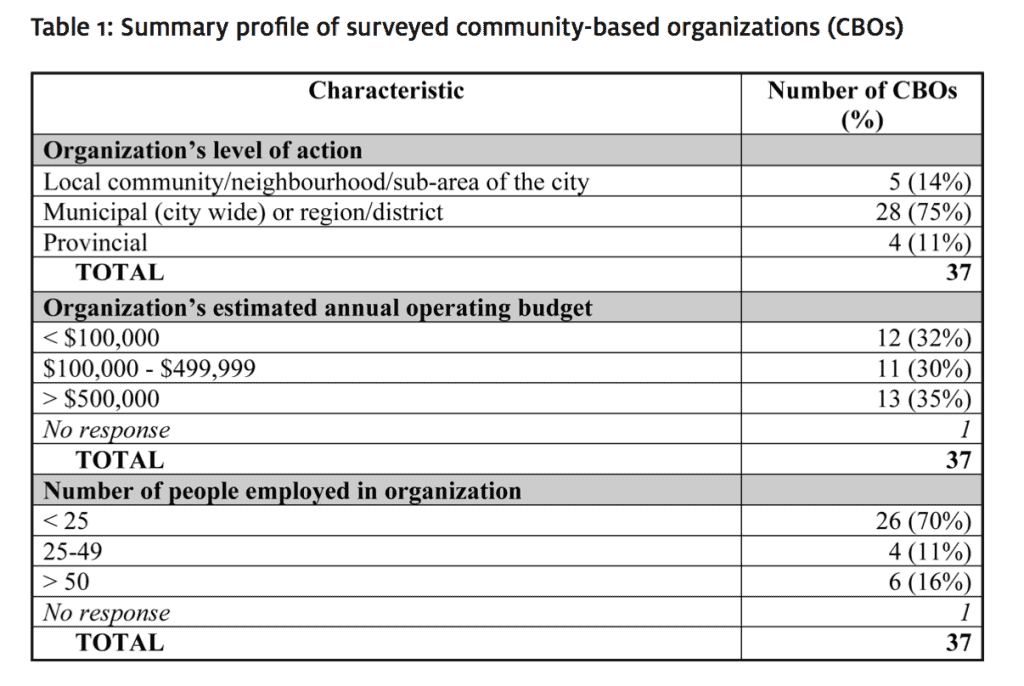
The specific research objective was to describe the determinants of health priorized by these organizations, which groups of people benefit, how these interventions are undertaken, who their partners are, and how they are funded. A qualitative, semi-structured survey research design was adopted. A convenience sample (Berg, 2004) using the Regina RIC membership e-list was generated; there were 169 discrete individuals, organizations (local, regional/district, municipal, provincial and federal), networks, and community associations represented on the e-list. Members of the Regina RIC e-list were invited to participate in the on-line survey via an email letter; a reminder message was sent out four weeks later. Thirty-seven nonprofit organizations participated in the study for a response rate of 22%. Table 1 offers a summary profile of the sample.
table 1: summary profile of surveyed community-based organizations (CBOs)
The unit of analysis was each initiative delivered by each organization; 77 initiatives were reported on. Initiatives were defined as services or projects with specific activities delivered to groups of people in need over a specified period; thus, organizations were not asked to report on entire programs run by their agencies. An on-line, self-administered survey included 12 specific questions about each initiative (e.g., name of the initiative, initiative mandate, target populations, geographic scale of service delivery, main partners, key activities, estimated operating budget, major sources of funding, the top four determinants of well-being addressed by the initiative) and five general questions about participants’ organizations (e.g., mandate, size, geographic focus, annual operating budget, funders). Organizations were asked to report on a maximum of four initiatives that they had implemented to improve the well-being of their communities. The survey took, on average, one hour to complete. Content analysis, which relies on summaries, explanations and frequency counts, was the analytic method used on these data (Berg, 2004; Titscher, Meyer, Wodak, & Vetter, 2007). Ethics approval was sought and granted by the University of Regina Research Ethics Review Board.
There were research limitations. First, given there is not one central database of nonprofit organizations representing the universe of agencies, we cannot say in what ways our sample compares and contrasts with such a universe. Second, given the online nature of the survey, we do not have any way to validate respondents’ interpretations of the questions or their subsequent responses. Third, our sample was biased in favour of organizations that understood and/or worked with the determinants of health, understood the population health definitions and instructions, had some computer and internet/online surveys skills, and were already on the Regina RIC email list.
Results
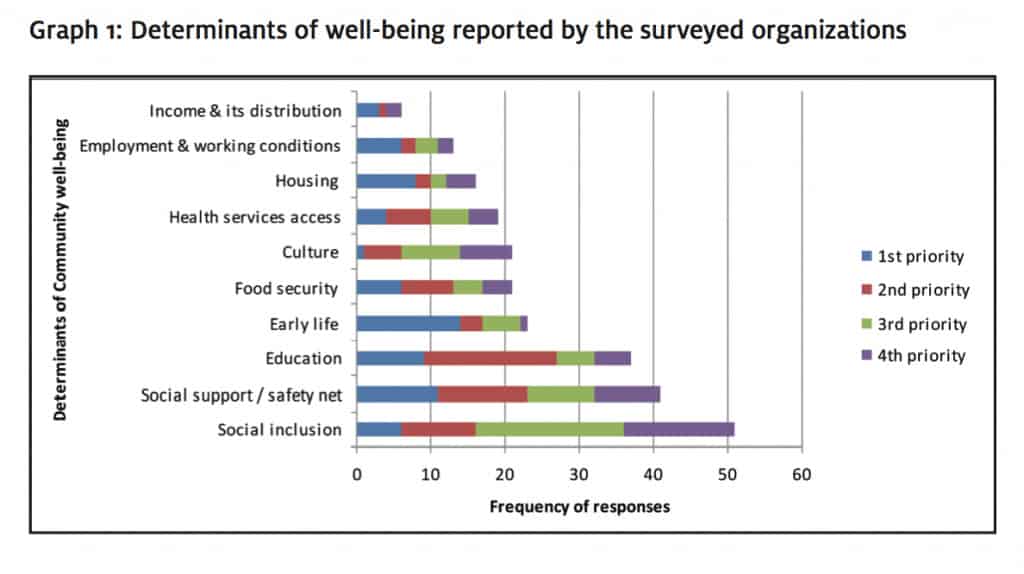
The 37 organizations reported a total of 77 initiatives. The main survey question was, “Which determinants of community well-being are the top four priorities in this initiative?” The organizations characterized their initiatives by determinants of well-being in order of priority. Graph 1 presents a summary of these data. The determinants that received the highest cumulative score across all four priorities were social inclusion (frequency of 51), social support/social safety net (frequency of 41), and education (frequency of 38). The determinant that received the lowest score was income and its distribution.
graph 1: determinants of well-being reported by the surveyed organizations
The organizations were asked, “What is this initiative’s target population?” Respondents noted the age groups and sex of their program participants; they were permitted to check more than one category. The results indicate that for the majority of initiatives, both sexes tended to be served, but for some initiatives, women were the sole beneficiaries. Young adults aged 19-24 years were the most frequently served by these initiatives (N=54), followed closely by youth aged 13-18 years (N=51) and then adults aged 25-64 years (N=50).
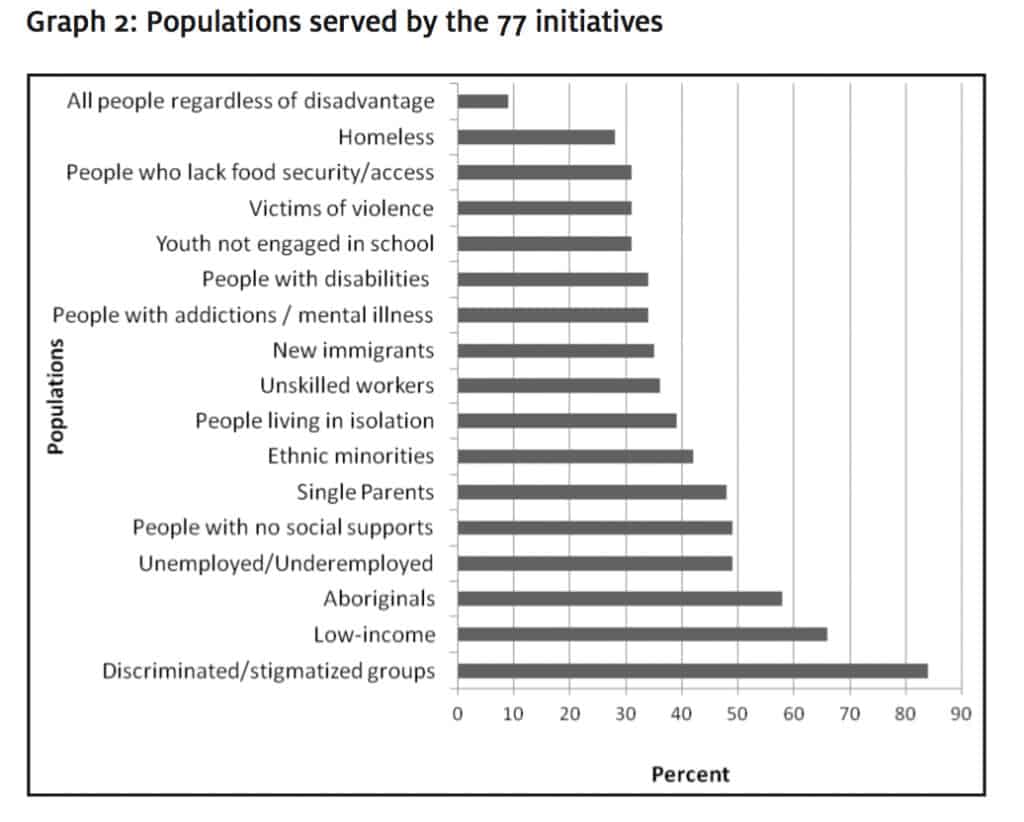
Organizations were also asked, “What best describes the target population of this initiative?” Organizations had to indicate which groups were the focus of their initiatives; they were encouraged to check off multiple responses if they fit. Graph 2 shows the populations served by the 77 initiatives. The most frequently cited response was “discriminated/stigmatized groups.” The least cited response was “all people regardless of disadvantage.” It is noteworthy that many of these categories are not mutually exclusive; for example, Aboriginal peoples often face discrimination, thus they could have been included in two categories; thus, caution should be exercised when thinking about these results.
graph 2: Populations served by the 77 initiatives
The organizations were asked, “What are this initiative’s key activities?” Answers to this question help us to better understand the depth of these initiatives. The most common 10 activities offered by the initiatives include the following (note: initiatives could have more than one activity):
• opportunities for social support/networking (43/77, 56%),
• community engagement and community development (37/77, 48%),
• education (36/77, 47%),
• peer support (29/77, 38%),
• physical activity/recreation (29/77, 38%),
• food security/access (22/77, 29%),
• cultural engagement (18/77, 23%),
• public safety (15/77, 19%),
• safe affordable housing/shelter (13/77, 17%),
• early childhood development (13/77, 17%).
The least cited activity was income security (1/77); this is not a surprise because income security is the responsibility of governments and this is a list of activities offered through these nonprofit organizations.
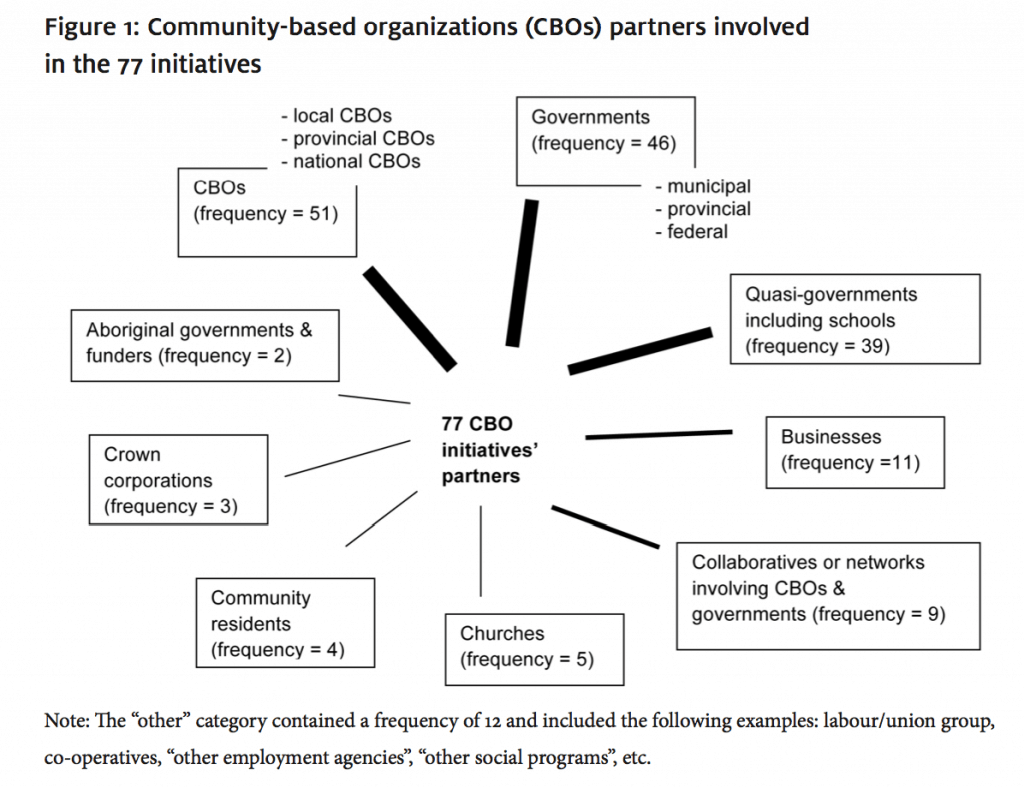
Organizations were asked, “For this initiative, who are your main partners?” Figure 1 offers a schematic representation of the 77 initiatives and their partners. Respondents were permitted to list up to six partners. The challenge with these data is that some respondents explicitly stated organizations’ names (e.g., Regina Food Bank) while others spoke about their partners in generalities (e.g., nonprofit organizations). Thus, Figure 1 presents these data in more general terms. In general, 13/77 (17%) of the initiatives listed one partner while the majority of initiatives had three or more partners.
figure 1: community-based organizations (CBOs) partners involved in the 77 initiatives
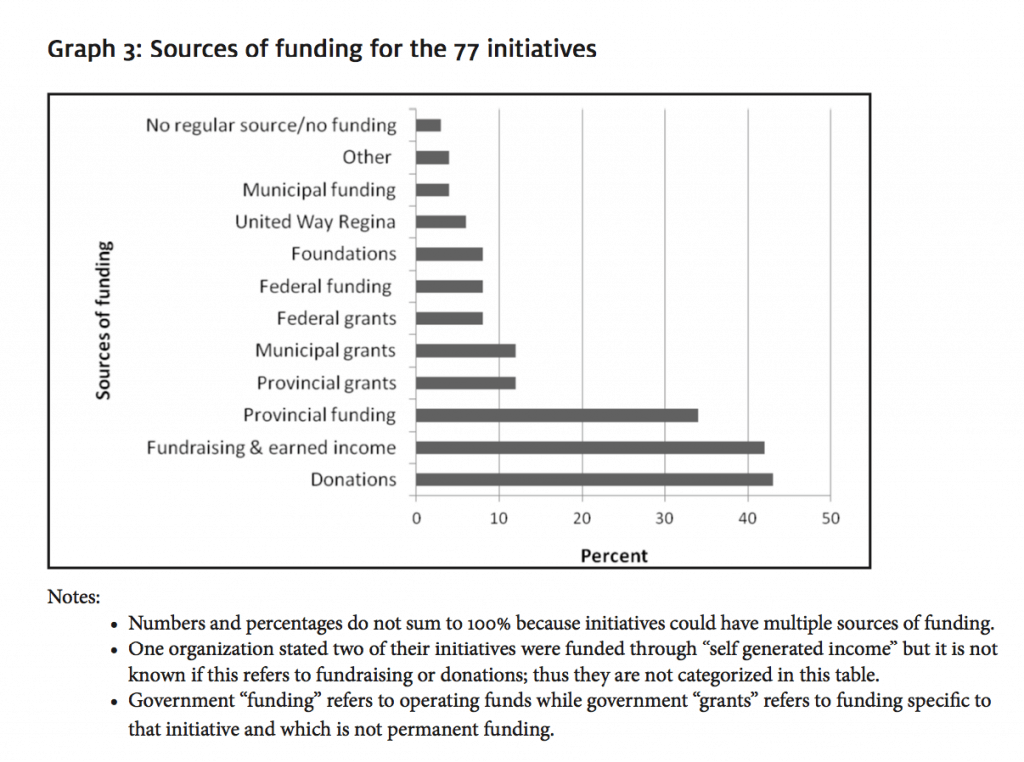
The organizations were also asked, “What is this initiative’s major sources of funding?” Respondents were permitted to check more than one source of funding. The different sources of funding are shown in Graph 3. The most frequently cited source of funding for these 77 initiatives was donations (33/77, 43%), followed closely by fundraising and earned income (32/77, 42%).
graph 3: sources of funding for the 77 initiatives
The organizations were also asked, “What is this initiative’s estimated annual operating budget?” The largest number of initiatives (N=34) had annual operating budgets below $50,000. Collectively, these 34 initiatives had between one and four funding sources (with one funding source being the most common response). The most frequently cited sources of funding were donations and fundraising/earned income for these smaller initiatives. A second group of initiatives (N=24) had annual operating budgets of more than $200,000. These 24 initiatives had between one and four funding sources (with two or three funding sources being the most common response). Donations, fundraising/ earned income, and provincial funding were the top three funding sources in initiatives operating on more than $200,000 per year.
Conclusions
Determinants of well-being addressed by a sample of community-based organizations
This sample of organizations is working on a variety of determinants of community well-being. The most frequently chosen determinant in the sample was social inclusion; social inclusion refers to processes that engage individuals and groups so they can participate fully in their communities, for example, in the labour force, in leisure and recreational opportunities, and in educational opportunities. Social inclusion/exclusion is recognized as an important determinant of health in much of the literature (Loppie Reading & Wien, 2009; Raphael, 2009). The key activities these organizations offer through their initiatives reflect their work on social inclusion; the two most frequently cited activities were social support activities and community engagement activities. Social inclusion can be viewed as a cross-cutting theme that is found embedded in numerous other determinants of well-being (e.g., low income, employment). Literature and theories about the salience of the social variables and social processes abound (see, for example, Bouchard, Roy, & van Kemenade, 2006; Brunner & Marmot, 2006; Kawachi, Kennedy, & Glass, 1999). Indeed, some research shows social inclusion can reduce health inequities (Baum, Newman, Biedrzycki, & Patteron, 2010).
conclusion #1: Community-based organizations are working on a variety of determinants of community well-being but with a tendency toward services and activities that reflect an emphasis on the social context, social supports, and community engagement. Thus, these organizations are naturally implicated in population health work, given that these social elements are known to influence both individual and community health. Interestingly, mainstream media tend to report on surgery wait lists and hospital underfunding more than the determinants of health, thus the general public tends to not know about this situation.
Further, the analysis shows that approximately 90% of initiatives were intended for specific marginalized populations. The organizations’ most frequently cited populations served were groups who experience discrimination and/or are stigmatized. Two observations about these results may be offered. First, given that approximately 90% of the initiatives are intended to serve populations with various vulnerabilities, they are targeted and not intended to be universal. This result has been reported in other research: “Programs are tailored to the particular needs of the community … In so doing, community organizations create a safety net for the most vulnerable …” (Danaher, 2011, p. 4).
Second, a greater number of respondents chose discrimination as a central identifier, which may indicate a collective perception of its salient impact on people’s well-being. Discrimination can be described as negative judgements about certain groups of people due to their characteristics (e.g., skin colour, economic status, age, disability) that results in limited access to the necessities of life (e.g., food, shelter, health care). Discrimination is identified as a determinant of health in the scholarly literature (Loppie Reading & Wien, 2009; McGibbon, 2012) and is a multi-dimensional concept directly tied to exclusion (Galabuzi, 2004); discrimination transforms “the experience of inequality into powerlessness, hopelessness and despair,” all of which have negative emotional and physical impacts on health (Galabuzi, 2004, p. 247).
It is important to understand the multi-dimensional nature of discrimination. Health experts have come to understand there are many and intersecting systems that operate to keep certain groups of people marginalized. For example, many categories of social identity (e.g., race, class, gender) actually melt together and result in a new social status, that is not impacted simply by racism, or by classism, or by sexism (Hankivsky & Christoffersen, 2008; McGibbon, 2012). To complicate this further, we know from Aboriginal health scholars that many and intersecting systems of discrimination are connected to “life stages, socio-political contexts and social determinants of health [that are] nested spheres of origin, influence and impact” resulting in many different pathways to health (Loppie Reading & Wien, 2009, p. 25). This leads us to a public policy challenge: to conceive and implement public policies that embrace these intersecting and dynamic spheres of health influences. For example, it is not enough to simply formulate a good, provincial government poverty reduction policy based on incomes, but rather, such a policy requires supportive mechanisms as well as flexibility to accommodate differences across groups with diverse life experiences, otherwise such policies simply contribute to population illness.
conclusion #2: These organizations offer targeted services to marginalized populations with the recognition that discrimination and exclusion—multidimensional concepts—are more telling and potent than racism or classism alone, for example. Thus, given nonprofit organizations’ front-line work in communities, they are well-positioned to help inform health and social policy makers about the multi-dimensional nature of discrimination and the need to discern how to handle these dynamic and intersecting spheres of health influences and the accompanying public policy and program requirements. However, despite significant cross-departmental, provincial government restructuring in Saskatchewan, there is not widespread engagement and participation of nonprofit, social service organizations in systems planning toward this end (see, for example, the Senior Inter-ministry Steering Committee and Regional Intersectoral Committees spread across the province).
Now let us consider how these initiatives focusing on the determinants of well-being are financially supported. In general, these organizations’ initiatives were most frequently funded by donations, fundraising, and earned income (e.g., sale of products, fees-forservice), and provincial funding (in descending order). It is not surprising to observe a high occurrence of donations and fundraising/earned income because these are characteristic of the nonprofit sector. There has been a documented shift in funding models over the past two decades in Canada wherein nonprofit organizations now typically rely on multiple funding sources including donations, fees for service, fundraising and multiple, often short-term, government sources because of a shift away from core funding (Hall, Andrukow, Barr, Brock, de Wit, et al., 2005; Scott, 2003). If the determinants of well-being are such important ingredients in building healthier communities, it is not appropriate that initiatives directed at enhancing these determinants are relying on the generosity of others for charitable donations and/or require organizations to engage in a multitude of fundraising activities. In addition, given some initiatives are funded through short-term government “grants,” their continuation is precarious.
conclusion #3: Given that community-based organizations are central players in work on the determinants of well-being, and given that work on these determinants is central to creating healthier communities, current funding models require reconfiguration to include more sustainable program funding derived from the tax system and not from peoples’ acts of charity. The health of populations should not depend on charitable acts. Therein lies a critical point raised earlier: if we as a society are to make progress on reducing health inequities, the restructuring of the welfare state in Canada requires a clearly defined relationship between governments and the nonprofit sector—including a commitment to stabilizing and sustaining the sector.
Further collaborative action
The second purpose of the Regina RIC Team’s project was to catalyze further collaboration and action on the determinants of well-being. To this end, respondents were also asked who their collaborative partners were for these initiatives. The majority stated they have multiple partners with other nonprofit organizations, quasi-governmental organizations, governments, and networks; only 13/77 (17%) of the initiatives had just one partner. There are not enough detailed data collected for this study to state unequivocally, but cross-organization communication and degrees of service integration exist in this sample. Additional research should focus on more detailed examination of the number and nature of partnerships in determinants of health initiatives given the importance of cross-sectoral action required to move toward greater health equity in communities (Daghofer & Edwards, 2009; Johnson et al., 2008).
conclusion #4: This sample of community-based organization is working collaboratively with other community organizations, governments and the private sector—not in isolation—on the determinants of health. Making the survey data inventory publicly and freely available, possibly through the public library or 211 websites, will provide all organizations with the opportunity to find each other and further build collaborative initiatives on the determinants of health.
These human service integration findings are in line with a direction set in Saskatchewan more than a decade ago and continue today. Human services integration and the key structures to advance work on the determinants of health are reflected in the formation of the provincial government’s Senior Inter-ministry Steering Committee, formerly the Human Services Integration Forum, and Regional Intersectoral Committees (RICs) across the province. This restructuring is viewed as a step in the right direction given both Canadian and international literature cite the importance of cross-sectoral, cross-departmental, and integrated human service planning and delivery for enhancing population health and reducing health inequities (Daghofer & Edwards, 2009; Health Council of Canada, 2010; Johnson et al., 2008; WHO Commission on the Social Determinants of Health, 2008)—with the caution drawn earlier in conclusion #2 that in general, nonprofit organizations do not figure prominently in this restructured reality. The determinants of well-being framework adopted by the Regina Regional Intersectoral Committee in 2009 in particular, places it in an optimal position to have an impact on health inequities. What is unclear are the actual (i.e., real) impacts of these government restructuring and priority setting exercises on the health of marginalized communities.
conclusion #5: Community-based organizations are working on the determinants of health, but the challenge is to ensure that these determinants continue to be policy and program priorities for governments, especially if we are to reduce health inequities in Saskatchewan. As these organizations continue to be pressed to measure their impacts, so should the provincial government measure the actual impacts of these new horizontal and vertical structures on population health and health inequities.
In closing, this sample of community-based organizations is working on a variety of determinants of health, serving a variety of vulnerable populations and age groups, offering myriad activities, funded by diverse sources and carried out with multiple organizational partners. Nonprofit social service organizations are naturally implicated in population health, given their work on the determinants of health. All of this is good news. However, there is cause for concern given that the nonprofit system currently at work on the determinants of health is precariously situated and inequities in health persist across communities. The way forward to reduce health inequities requires us to develop a stable and sustainable nonprofit social service sector, a coherent and explicit framework for carefully planned work on the determinants of health involving an intentionally defined relationship between governments and nonprofit organizations, and public policies informed by these organizations’ front-line work on the dynamic and intersecting spheres of health influences.
Acknowledgements
The author wishes to express her appreciation for the contributions made by Carla Bolen Anderson, formerly of the Regina Qu’Appelle Health Region, and Wendy Stone of the Regina Police Service in the preparation of the full report available at http://www.spheru.ca/. A note of appreciation is also extended to Dr. Tom McIntosh and Dr. Bonnie Jeffery, SPHERU, University of Regina, for their insightful comments on earlier drafts of this article.
Notes
1. The Regina Regional Intersectoral Committee (RIC) is a cross-provincialgovernment department committee comprising representatives from seven provincial government ministries, school boards, the health region, the public library, Regina Police Service, the United Way, Service Canada, the university, and the local college.
2. To view a full copy of the research report, please go to http://www.spheru.ca/publications/files/Orgs%20work%20on%20Regina%20SDOHs%20FINAL.pdf .
References
Bakker, Isabella, & Scott, Katherine. (1997). From the postwar to the post-liberal Keynesian welfare state. In W. Clement (Ed.), Understanding Canada: Building on the New Canadian Political Economy (pp. 286–310). Kingston, ON: McGill-Queen’s University Press.
Baum, Fran, Newman, Lareen, Biedrzycki, Katherine, & Patterson, Jan. (2010). Can a regional government’s social inclusion initiative contribute to the quest for health equity? Health Promotion International 25(4), 474–482.
Berg, Bruce L. (2004). Qualitative research methods for the social sciences. Boston, MA: Pearson Education Inc.
Bolen, Carla, & Ramsay, Doug. (2008). From concept to action: A social determinants of health workplan. Regina, SK: Regina Qu’Appelle Health Region, Mental Health and Addiction Services.
Bouchard, Louise, Roy, Jean-Francois, & van Kemendae, Solange. (2006). An analysis of social capital and health using a network approach: Findings and limitations. Horizons: Policy Research Initative, Government of Canada 8(2), 71–74.
Broad, Dave, & Antony, Wayne. (1999). Citizenship and social policy: Neo-liberalism and beyond. In D. Broad & W. Antony (Ed.), Citizens or Consumers? Social Policy in a Market Society (pp. 9–19). Halifax, NS: Fernwood Publishing.
Brock, Kathy, Ed. (2002). Improving connections between governments and nonprofit and voluntary organizations: Public policy and the third sector. Kingston, ON: McGill-Queen’s University Press.
Brock, Kathy, & Banting, Keith (Eds.). (2001). The nonprofit sector and government in a new century. Kingston, ON: McGill-Queen’s University Press.
Brooks, Neil. (2001). The role of the voluntary sector in a modern welfare state. In Jim Phillips, B. Chapman & D. Stevens (Eds.), Between State and Market: Essays on Charities Law and Policy in Canada (pp. 166–216). Kingston, ON: McGill-Queen’s University Press.
Browne, Paul Leduc. (1996). Love in a cold world: The voluntary sector in an age of cuts. Ottawa, ON: Canadian Centre for Policy Alternatives.
Brunner, Eric, & Marmot, Michael. (2006). Social organization, stress and health. In M. Marmot & R. G. Wilkinson (Eds.), Social Determinants of Health (pp. 6–30). New York, NY: Oxford University Press.
Burke, Mike, Mooers, Colin, & Shields, John. (2000). Introduction: Critical perspectives on Canadian public policy. In M. Burke, C. Mooers, & J. Shields (Eds.), Restructuring and Resistance: Canadian Public Policy in an Age of Global Capitalism (pp. 11–23). Haifax, NS: Fernwood Publishing.
Canadian Welfare Council. (1938). A study of community welfare services in Saskatoon: Part I of a report of a survey made by the Canadian Welfare Council for the Community Council of Saskatoon. Ottawa, ON: Council House.
Daghofer, Diana, & Edwards, Peggy. (2009). Toward health equity: A comparative analysis and framework for action (working document). Ottawa, ON: Strategic Initiatives and Innovations Directorate, Public Health Agency of Canada.
Danaher, Audrey. (2011). Reducing disparities and improving population health: The role of a vibrant community sector. URL: http://www.wellesleyinstitute.com/publicationpapers/reducing-disparities-and-improving-population-health-the-role-of-a-vibrantcommunity-sector (September 5, 2011).
Elson, Peter. (2011). High ideals and noble intentions: Voluntary sector-government relations in Canada. Toronto, ON: University of Toronto Press.
Galabuzi, Grace-Edward. (2004). Social exclusion. In D. Raphael (Ed.), Social Determinants of Health: Canadian Perspectives (pp. 235–251). Toronto, ON: Canadian Scholars’ Press Inc.
Government of Canada, Voluntary Sector Initiative. (2002). A code of good practice on policy dialogue: Building on an accord between the government of Canada and the voluntary sector. Ottawa, ON: Privy Council of Canada.
Hall, Michael, Andrukow, Alison, Barr, Cathy, Brock, Kathy, de Wit, Margaret, Embuldeniya, Don, John, Louis, Lasby, David, Levesque, Benoit, Malinksy, Eli, Stowe, Susan, & Vaillancourt Yves. (2005). The capacity to serve: A qualitative study of the challenges Ffcing Canada’s nonprofit and voluntary organizations. Toronto, ON: Canadian Centre for Philanthropy.
Hall, Michael, & Banting, Keith. (2000). The non-profit sector in Canada: An introduction. In K. Banting (Ed.), The Nonprofit Sector in Canada: Roles and Relationships (pp. 1–28). Kingston, ON: McGill-Queen’s University Press.
Hall, Michael, de Wit, Margaret, Lasby, David, McIver, David, Evers, Terry, Johnston, Chris, McAuley, Julie, Scott, Katherine, Cucumel, Guy, John, Louis, Nicol, Richard, Berdahl, Loleen, Roach, Rob, Davies, Ian, Rowe, Penelope, Frankel, Sid, Brock, Kathy, & Murray, Vic. (2004). Cornerstones of community: Highlights of the National Survey
of Nonprofit and Voluntary Organizations. Ottawa, ON: Ministry of Industry, Statistics Canada, Catalogue No. 61-533-XIE. URL: http://library.imaginecanada.ca/files/nonprofitscan/en/nsnvo/nsnvo_report_english.pdf (June 1, 2012).
Hancock, Trevor, Labonte, Ronald, & Edwards, Rick. (2000). Indicators that count! – Measuring population health at the community level. Toronto, ON: Centre for Health Promotion at University of Toronto and ParticipACTION.
Hankivsky, Olena, & Christoffersen, Ashlee. (2008). Intersectionality and the determinants of health: A Canadian perspective. Critical Public Health 18,(3), 271–283.
Hanlon, Neil, Rosenberg, Mark, & Clasby, Rachel. (2007). Offloading social care responsibilities: Recent experiences of local voluntary organizations in a remote urban centre in British Columbia, Canada. Health and Social Care in the Community 15(4), 343–351.
Health Council of Canada. (2010). Stepping it up: Moving the focus from health care in Canada to a healthier Canada. Toronto, ON: Health Council of Canada.
Johnson, Shanthi, Abonyi, Sylvia, Jeffery, Bonnie, Hackett, Paul, Hampton, Mary, McIntosh, Tom, Martz, Diane, Muhajarine, Nazeem, Petrucka, Pammla, & Sari, Nazmi. (2008). Recommendations for action on the social determinants of health: A Canadian perspective. The Lancet 372, 1690–1693.
Kawachi, Ichiro, Kennedy, Bruce, & Glass, Roberta. (1999). Social capital and self-rated health: A contextual analysis. In I. Kawachi, B. Kennedy, & R. Wilkinson (Eds.),
The Society and Population Health Reader: Income Inequality and Health (pp. 236–248). New York, NY: The New Press.
Labonte, Ronald, Muhajarine, Nazeem, Abonti, Sylvia, Woodard, Georgia Bell, Jeffery, Bonnie, McCubbin, Michael, & Williams, Allison. (2002). An integrated exploration into the social and environmental determinants of health: The Saskatchewan population health and evaluation research unit. Chronic Diseases in Canada 23(2).
Lemstra, Mark, & Neudorf, Cory. (2008). Health disparity in Saskatoon: Analysis to intervention. Saskatoon, SK: Saskatoon Health Region.
Loppie Reading, Charlotte, & Wien, Fred. (2009). Health inequalities and social determinants of aboriginal people’s health. Prince George, BC: National Collaborating Centre for Aboriginal Health.
Marmot, Michael, & Wilkinson, Richard G. (Eds.). (2006). Social determinants of health. New York, NY: Oxford University Press.
McGibbon, Elizabeth. (2012). People under threat: Health outcomes and oppression. In E. McGibbon (Ed.), Oppression: A Social Determinant of Health (pp. 32-44). Winnipeg, MB: Fernwood.
Mulvale, James. (2001). Reimagining social welfare: Beyond the Keynesian welfare state. Aurora, ON: Garamond Press.
O’Sullivan, Michael, & Sorensen, Sandra. (1988). Saskatchewan. In J. Ismael & Y. Vaillancourt (Eds.), Privatization and Provincial Social Services in Canada: Policy, Administration and Service Delivery (pp. 75-93). Edmonton, AB: University of Alberta Press.
Phillips, Susan. (2009). The Harper government and the voluntary sector: Whither a policy agenda? In R. Laforest (Ed.), The New Federal Policy Agenda and the Voluntary Sector (pp. 7-34). Kingston, ON: McGill-Queen’s University Press.
Raphael, Dennis. (Ed.). (2009). Social determinants of health: Canadian perspectives. Toronto, ON: Canadian Scholars’ Press
Rice, James, & Prince, Michael. (2003). Changing politics of Canadian social policy. Toronto, ON: University of Toronto Press.
Scott, Katherine. (2003). Funding matters: The impact of Canada’s new funding regime on nonprofit and voluntary organizations [Electronic Resource]. URL: http://www.ccsd. ca/pubs/2003/fm/index.htm (Sept. 2, 2009).
Shragge, Eric, & Fontan, Jean-Marc. (2000). Social economy: International debates and perspectives. Montreal, QC: Black Rose Books.
Teeple, Gary. (2000). Globalization and the decline of social reform: Into the twenty-first Century. Aurora, ON: Garamond Press.
Thériault, Luc, Gill, Carmen, & Kly, Yussuf. (2002). Personal social services and the third sector in Saskatchewan. In Y. Vaillancourt, L. Tremblay and translated by Stuart Anthony Stilitz (Eds.), Social Economy: Health and Welfare in Four Canadian Provinces (pp. 135-161). Halifax, NS: Fernwood Publishing and LAREPPS, École de travail social, Université du Québec a Montréal.
Titscher, Stefan, Meyer, Michael, Wodak, Ruth, & Vetter, Eva. (2007). Methods of text and discourse analysis: In search of meaning. London, UK: Sage Publications Ltd.
Tremblay, Louise, Aubry, Francois, Jetté, Christian, & Vaillancourt, Yves. (2002). Introduction. In Y. Vaillancourt, L. Tremblay and translated by Stuart Anthony Stilitz (Eds.), Social Economy: Health and Welfare in Four Canadian Provinces (pp. 19-25). Halifax, NS: Fernwood Publishing and LAREPPS École de travail sociale, Université du Québec à Montréal.
WHO Commission on the Social Determinants of Health. (2008). Closing the gap in a generation: Health equity through action on the social determiants of health: Final report. Geneva: World Health Organization.
Wilkinson, Richard, & Marmot, Michael (Eds.). (2003). Social determinants of health: The solid facts. Denmark: World Health Organization.
Young, T. Kue. (2005). Population health: Concepts and methods. New York, NY: Oxford University Press.
Gloria DeSantis is Research Associate at the Saskatchewan Population Health and Evaluation Research Unit, University of Regina, 3737 Wascana Pkwy, Regina, SK, Canada, S4S 0A2. Email: gloria.desantis@uregina.ca .